Primitive NeuroEctodermal tumors (PNETs):
Primitive neuroectodermal tumour or PNET belong to a group of tumours characterized by hypercellular arrangement of “Small blue Cell tumours” or SBCT.
These "SBCT" cells have:
- Pronounced nuclear features but very little cytoplasm
- “Nuclear molding” and “cell wrapping”
These features are the result of overwhelming cellularity and the intrinsic biophysical phenotype of the tumour cell.
As a general category, SBCT encompasses:
- hematolymphoid tumurs
- small cell carcinomas
- neuroendocrine tumours
- PNET
Obviously, the location of the lesion dictates further fine-tuning of the differential diagnosis. Additional histological features such as “pale islands” in medulloblastomas are invaluable in formulating the final diagnosis.
In the central nervous system, PNETs are grade IV/IV tumour with undifferentiated or poorly- differentiated neuroepithelial cells and the capacity for divergent differentiation along neuronal, astrocytic, ependymal, mesenchymal, and melanocytic lines1. The presence of “pale islands” in medulloblastomas is an example of focal divergent astrocytic differentiation.
Supratentorial PNETs are histologically indistinguishable from infratentorial PNETs i.e. medulloblastomas. They tend to behave more aggressively than medulloblastomas and often present with higher tumour burden at diagnosis (likely due to higher capacitance of the supratentorial cranial compartment) and are associated with higher incidence of disseminated disease at time of diagnosis2.
A significant number of supratentorial PNETs are located in close proximity to midline and functionally important structures such as the diencephalon (thalamus and hypothalamus) which restricts therapeutic options (surgery and RT). There is active research in the molecular differences between supra- and infratentorial PNET – which could be used as adjuncts in clinical diagnosis and as predictive molecular biomarkers3.
Classification of supratentorial PNETs and their reliable histological diagnosis in clinical practice remain a highly contentious topic amongst neuropathologists4 and one is directed to an amusing one pager by Peter Burger on the topic 5.
Practically, the presence of a SBCT, after ruling out other possibilities, composed of mainly undifferentiated neuroepithelial cells (immunopositive for synaptophysin and other markers) with focal divergent differentiation in a suprarentorial location is therefore classified as a supratentorial PNET.
Often, the regions of divergent differentiation, however minor, are invaluable in assisting in the “PNET” diagnosis.
One example is in differentiating between small cell glioblastoma and PNET without significant divergent differentiation and this example was again brought forth in Peter Burger’s article5. Briefly, the similarity in histology and the equally uninformative immunohistochemical profiles (probably secondary to the early/abnormal developmental status of the tumours) between the two tumours make definitive diagnosis extremely challenging. The clinical implication is that supratentorial PNET is much more prone to CSF spread along the neuraxis which might necessitate craniospinal RT. Also, the chemotherapeutic regimens are different for the two tumours. Lack of definitiveness in the pathological diagnosis often will have practical implications.
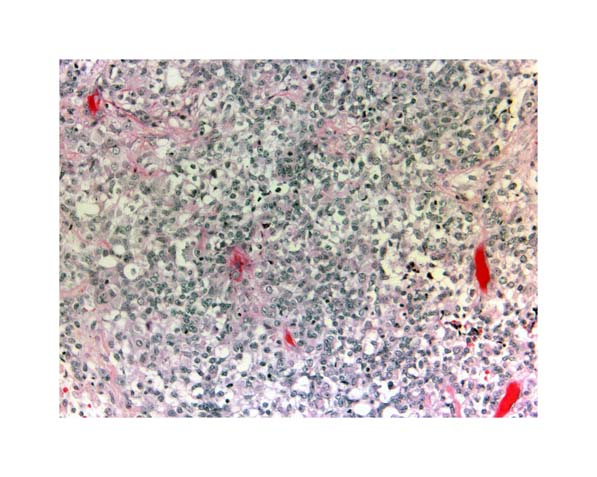
There is no discernable difference in the histology of infra and supratentorial PNET. These slides show a case of cerebellar large cell medulloblastoma with a suspicious focus of rhabdoid differentiation. This can be further investigated by a combination of IHC (INI1) and molecular genetic assays (22q FISH).These areas of divergent differentiation (along with the obvious large cell feature) are actually helpful in rendering a diagnosis of supratentorial PNET. Absence of these foci can make diagnosis of a supratentorial SBCT challenging eg.supratentiorial PNET vs small cell glioblastoma.

PATHOLOGY REFERENCES
1. Louis DN, Ohgaki H, Wiestler OD, et al: WHO Classification of Tumours of the Central Nervous System. Lyon, IARC, 2007
2. Jakacki RI: Pineal and nonpineal supratentorial primitive neuroectodermal tumors. Childs Nerv Syst 15:586-91, 1999
3. Li MH, Bouffet E, Hawkins CE, et al: Molecular genetics of supratentorial primitive neuroectodermal tumors and pineoblastoma. Neurosurg Focus 19:E3, 2005
4. Armstrong DD, Giangaspero F: Pediatric brain tumors: introduction. Brain Pathol 13:373-5, 2003
5. Burger PC: Supratentorial primitive neuroectodermal tumor (sPNET). Brain Pathol 16:86, 2006

