Introduction
Central nervous system tumors account for nearly 20 percent of all neoplasms in children under 15 years of age.
They are the second most common form of pediatric cancer, exceeded only by leukemia.
Brain tumors remain the leading cause of cancer deaths in pediatric oncology patients.
They differ from adult tumors in some important respects:
- A greater proportion of pediatric tumors are:
- Infratentorial
- Low grade gliomas (hemispheric high grade gliomas are rare in children)
- Gross total or near total excision has clearly been shown in many tumor types to improve prognosis.
- Treatment almost always involves a multidisciplinary team.
- On the whole, the long term prognosis is better in children than adults.
Incidence
The incidence of pediatric brain tumors is roughly 3.3 cases per 100,000 children in North America.
About 3000 children are diagnosed with brain tumors annually in the US.
About 30 children a year in British Columbia are diagnosed with a brain tumor.
Between 1973 and 1994, there was an increase in the reported incidence of childhood brain tumors. This coincided with the increased use of MRI imaging of the CNS which is likely to account for the perceived change in incidence.
From Canadian Cancer Statistics 2011:
In Canada:
Between 2003 and 2007, central nervous system (CNS) accounted for 16% of childhood cancer cases. During this time there were a total of 1,039 CNS cancers:
- 44% were astrocytomas
- 20% were intracranial and intraspinal embryonal tumors
- 10% were ependymomas
Approximately 27% of the deaths caused by childhood and youth cancers from 2002
to 2006 were secondary to CNS cancers.
For CNS cancers, the prognosis for astrocytoma (Five year OSP: 81%) was found to be higher than for intracranial and intraspinal embryonal tumors (Five year OSP: 58%). The great majority of astrocytomas in children are low grade.
(OSP = Observed survival proportions)
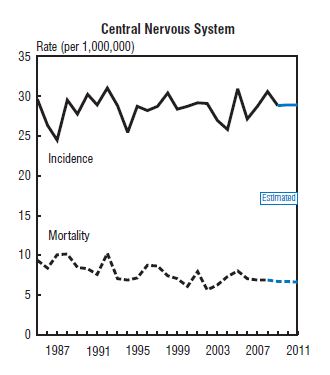
Age-Standardized Incidence and Mortality Rates for Central Nervous System Tumors in Children and Youth (0–19 Years), Canada, 1985–2011:
Age-Related Risk
Children under 5 years of age have the greatest incidence of brain tumors.
One third of all pediatric brain tumors present before the age of 5, and three-quarters before age 10.
Site of Origin
Roughly 60% of all childhood brain tumors are infratentorial and arise in the posterior fossa.
The most common of these are:
- Medulloblastoma
- Low-grade astrocytomas of the cerebellum
- Ependymomas
The frequency of specific types of brain tumors differs by cell type and age.
Relative Frequency of Pediatric Brain Tumors:
Relative Incidence of Common Brain Tumors in Children:
| Diagnosis | Relative Frequency |
Peak Age Group (years) |
Astrocytoma
|
35% |
2-10 |
Malignant glioma (anaplastic astrocytoma and glioblastoma multiforme) |
8% |
<1, >6 |
Brain stem glioma |
8% |
3-9 |
Oligodendroglioma |
2% |
<6 |
PNET (Medulloblastoma and supratentorial PNET) |
20% |
1-10 |
Ependymoma |
8% 3% 5% |
>6 |
Craniopharyngioma |
7% |
8-14 |
Pineal region and germ cell tumors |
4% |
<2, >6 |
Choroid plexus tumors |
2% |
<1 |
Others: ganglioglioma, meningioma, primitive embryonal tumors |
<2% each |
|
Summary of incidence characteristics for pediatric brain tumors:
| Annual incidence (Canada) | 217 |
Proportion of all childhood neoplasms |
20% |
Highest risk group |
<5 years old |
Proportion of cases presented <5 years of age |
30% |
Proportion of cases presented <10 years of age |
75% |
Most common site of origin |
Posterior fossa |
Most common histological subtype |
Astrocytoma |
Prognosis
The overall survival for children with pediatric brain tumors has improved in the past 10 to 20 years and is just over 70%.
This is most likely due to:
- Improved imaging/diagnosis
- Multidisciplinary approach
- Improved therapy
- Improved neurosurgical techniques and reduced peri-operative mortality
- Increasingly precise RT
- More intensive, multi-agent chemotherapy

