Pathology:
Pleomorphic xanthoastrocytomas are histologically WHO grade II.
Macroscopic Features:
- Generally superficial tumors attached to meninges.
- Frequently are cystic or forms a mural nodule in the cyst wall.
- Tumor may have an orange hue.
- Tumor firmer than adjacent brain tissue.
Microscopic Features:
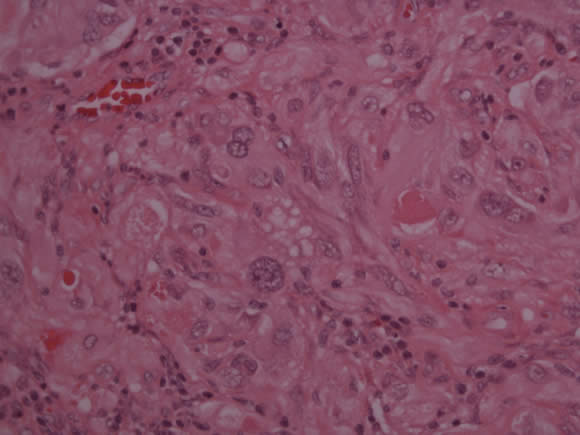
- Tumor cells are histologically variable. The tumor cells may be spindled, polygonal, mononuclear or multinucleated, and show marked variation.
- Cytoplasmic lipidization in tumor cells.
- Intranuclear inclusions are frequent.
- Eosinophilic granular bodies are present.
- Abundant reticulin fibers in the tumor which surrounds individual cells or groups of cells.
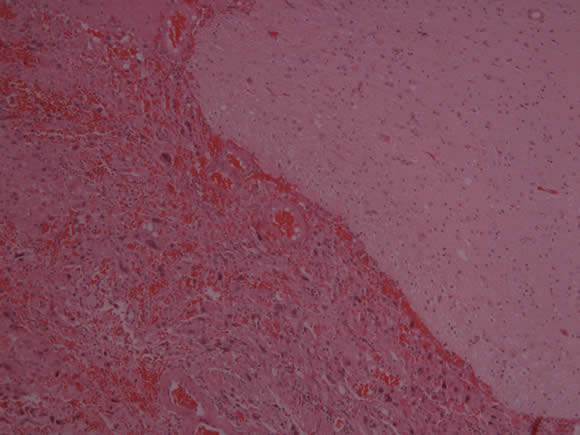
The slide below shows a pleomorphic xanthoastrocytoma with leptomeningeal involvement (bottom left).
The slide below shows a pleomorphic xanthoastrocytoma with variablility in tumor cell and nuclear size, lipidized cells and granular bodies.
Clinical Characteristics of Pleomorphic Xanthoastrocytoma (PXA):
Most Common Patient Age |
Late childhood/ adolescence |
Most Common Tumor Location |
Cerebral hemispheres |
Growth |
May infiltrate overlying meninges |
Histology |
|
Special Features |
Previously identified as JPAs, designated as a subtype within last 25 years |
Prognosis |
Good prognosis
Surgical cure possible |
These tumors may be cured by surgical resection and have a better prognosis than fibrillary astrocytomas. However:
- Tumor progression to anaplastic astrocytoma and glioblastoma forms has been described especially after radiotherapy treatment.
Malignant transformation of other low-grade astrocytomas occurs in less than 5% of cases. Once the tumor has progressed to a malignant form, it has a significantly worse prognosis.
If complete surgical resection is not feasible, radiation or chemotherapy may help with local control.
BRAF mutations have been detected in these tumors and this may have therapeutic implications.
Link:


