CT scan
Often when children first present with headache, vomiting and signs of raised intracranial pressure the first investigation to establish the diagnosis is a CT scan.
The CT below shows a midline posterior fossa tumor (#1) which proved to be a medulloblastoma.

- On non-contrast CT scans, medulloblastomas appear to have a homogeneous density, slightly greater than that of a normal brain. This helps to differentiate between:
- cerebellar astrocytomas - generally hypodense
- ependymomas - generally isodense
- Medulloblastomas are sometimes associated with large dense calcifications.
- Calcifications generally appear after treatment with radiotherapy, particularly in the brains of younger children as they are vulnerable to radiotherapy damage.
MR scan
Primary Tumor
On MR scan medulloblastomas usually appear as a contrast-enhancing midline or paramedian tumor.
- Large, well defined and usually midline solid tumor.
- Low to intermediate signal on T1 weighted MR
- Tumor grows to fill 4th ventricle - which becomes distorted and obliterated.
- Often extends to the cerebellopontine angles.
- Sometimes extend into the midbrain.
- Gadolinium enhancement is often heterogeneous.
- There may be necrosis, hemorrhage, or cystic changes (cystic or necrotic lesions also appear in 20-50% of cases).
- Unlike ependymomas they do not usually extend through the foramina of Luschka.
- Restricted diffusion on DWI (Diffusion Weighted Imaging)
See below for typical MR image of a midline medulloblastoma:
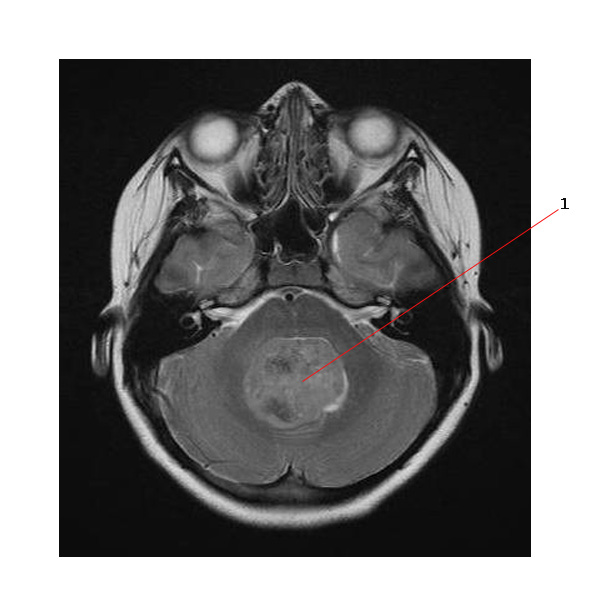
#1. Points to a large midline tumor filling the fourth ventricle. This is the same tumor shown in the CT image at the top of the page.
Below is a sagittal view of medulloblastoma (#3) on MR.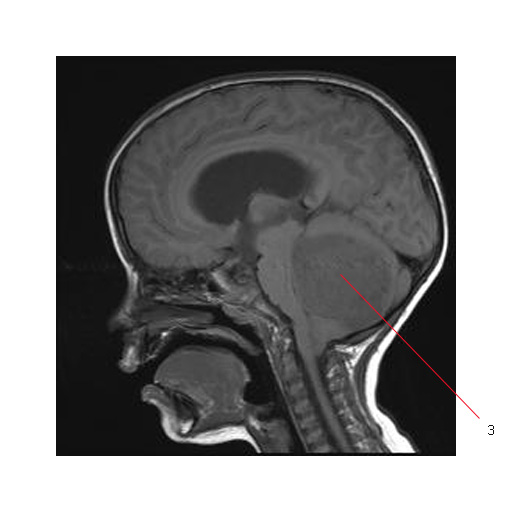
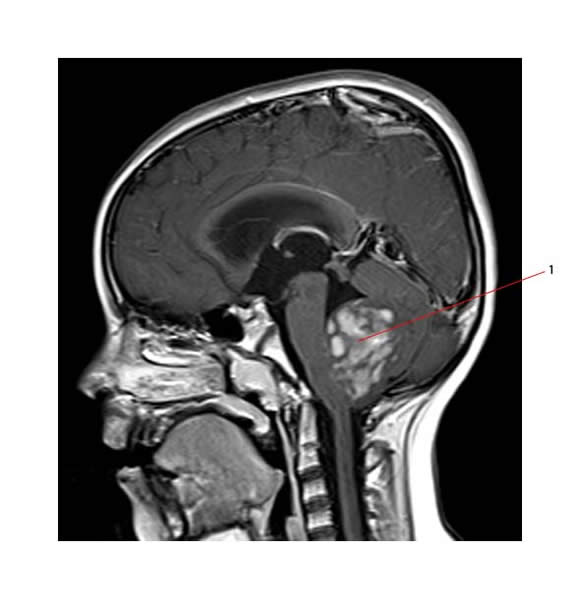
Medulloblastomas usually enhance with gadolinium Below is a MR (sag. T1, post gad) of a medulloblastoma (#1)
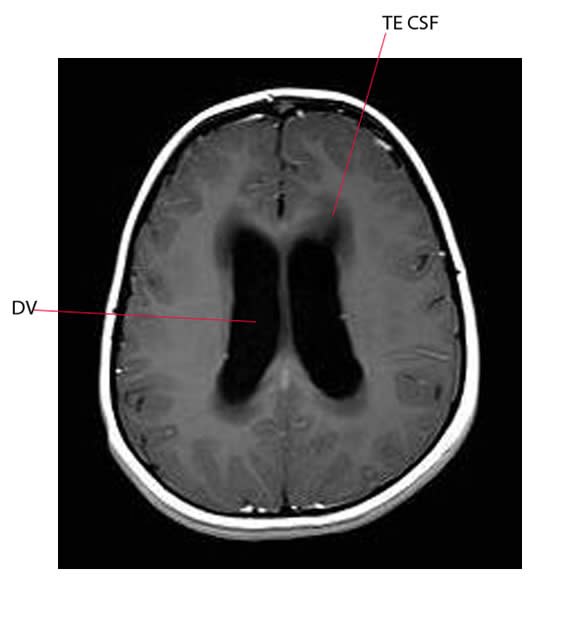
Hydrocephalus is usually present at diagnosis:
Below is a MR picture of hydrocephalus:
- DV points to dilated lateral ventricle
- TE CSF points to transependymal flow of CSF seen in the periventricular regions
Obliteration of the cisterns by a subarachnoid tumor may also occur, as well as progressive ventricular enlargement.
Metastatic Disease
Imaging of the entire neuraxis to detect the presence of metastatic spread to other sites in the CNS should always be done. Metastatic disease may cause enhancement in the ventricles, the spinal canal, or on the brain surface.
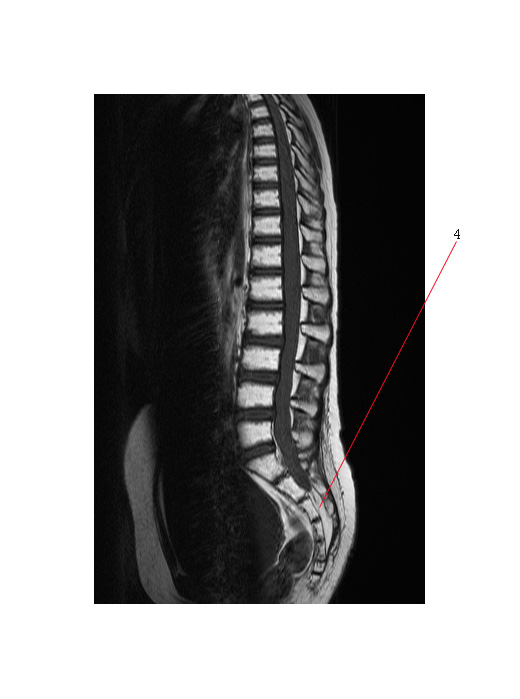
Spinal MR is the most sensitive method to evaluating spinal cord subarachnoid metastases (with gadolinium).
MRI of both the brain and spine for staging should be done before surgery. Post-operative staging MRI of the spine is inaccurate because of “false positives” if performed less than three weeks after surgery. This can result in delayed definitive therapy after resection
The MR below shows metastatic spinal disease from medulloblastoma. #4 points to disease filling the lower thecal sac.
Ultrasound Scan
- This is an effective imaging technique for the infant brain.
- The open fontanelles serve as acoustic windows.
- Neonatal skull is thin enough to allow transcalvanial sonography.
- Most tumors are hyperechoic relative to the normal brain.
Medulloblastoma can occasionally metastasize outside the central nervous system, especially to bone. A bone scan with plain film correlation as well as a bone marrow aspiration and biopsy may be useful in symptomatic patients or in those with abnormal blood cell counts at diagnosis. Aside from this routine bone scans are not required.
Link:


