History and Examination
A history and general physical examination (including complete neurological exam) should be performed.
Funduscopic Exam
- A funduscopic exam is likely to show increased intracranial pressure.
- 90% of patients will have papilledema at presentation.
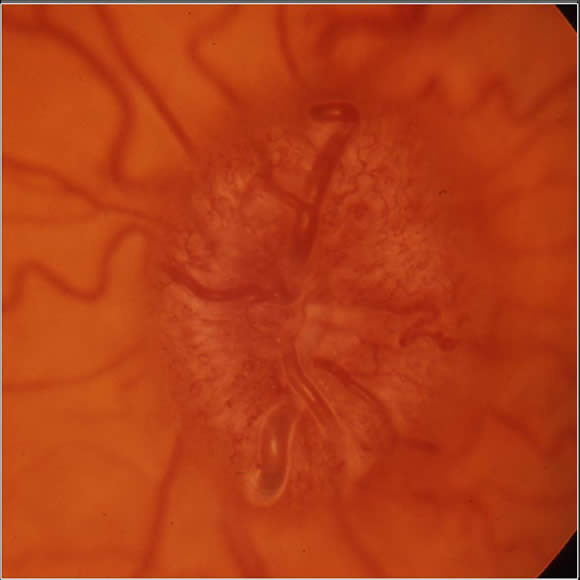
The photograph above shows papilledema (or papilloedema) - which is optic disc swelling caused by increased intracranial pressure.
CSF Cytology
- Cerebrospinal fluid (CSF) cytology is important to stage medullobastoma.
- Lumbar puncture is the most common method used for obtaining CSF.
- CSF should be obtained for CSF cytology via lumbar puncture a minimum of 7 days after surgery, to avoid false positive results.
- The gold standard would be to perform CSF staging via lumbar puncture 15 days after surgery.
Lumbar puncture in a child with raised intracranial pressure may precipitate herniation of the temporal uncus through the tentorium, compressing first the third nerve, then the midbrain, pons, medulla and finally the cerebellar tonsils and brain stem herniate through the foramen magnum. This can cause patient death.
- A ventricular drain that has been implanted may be used to obtain CSF, but these samples will contain malignant cells less often than samples obtained from the thecal sac.
-
It has also been suggested that CSF be obtained at the time of surgery from the cisterna magna for cytological analysis - but the significance of results in these circumstances is very questionable.
Below are medulloblastoma cells found in the cerebrospinal fluid (CSF obtained by lumbar puncture):
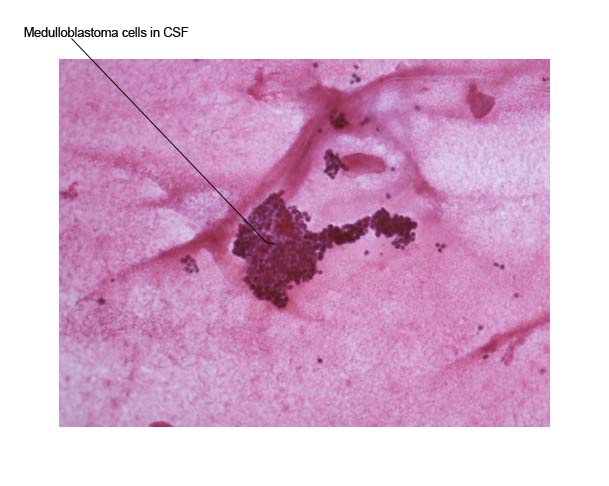 The slide above shows
metastatic cells in CSF, in sheets, clusters and singly.
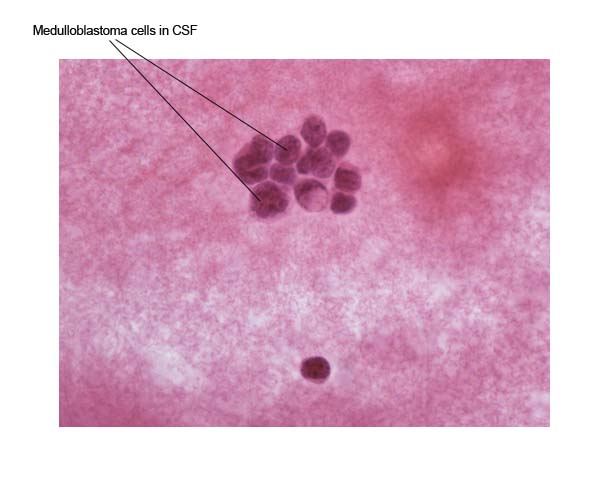
The slide above shows
metastatic cells in CSF, in sheets, clusters and singly.
The slide below again shows metastatic cells in CSF (higher magnification). The cells are atypical, have a high nuclear to cytoplasmic ratio and hyperchromatic nuclei.
Pre-operative imaging: Often a CT of the head is the first radiological investigation in a child who has symptoms and signs of a brain tumor.
MRI of both the brain and spine for staging should be done before surgery if at all possible. Post-operative staging MRI of the spine is inaccurate because of “false positives” if performed less than three weeks after surgery. This can result in delayed definitive therapy after resection.
Post-operative imaging: Post-operative MR should be performed of the brain and tumor resection cavity within 2 days of surgery to assess for possible residual disease.
Hemorrhage/post-surgical inflammation causes post-operative enhancement which is most prominent between 3 and 21 days after surgery. This makes the assessment of metastatic disease difficult.

