Transcriptional profiling studies of medulloblastoma tumors have shown multiple
distinct molecular subgroups with different:
- Demographics
- Transcriptomes
- Somatic genetic events
- Clinical outcomes
Classification outlined in a manuscript produced as a result of a consensus conference held in Boston 2010:
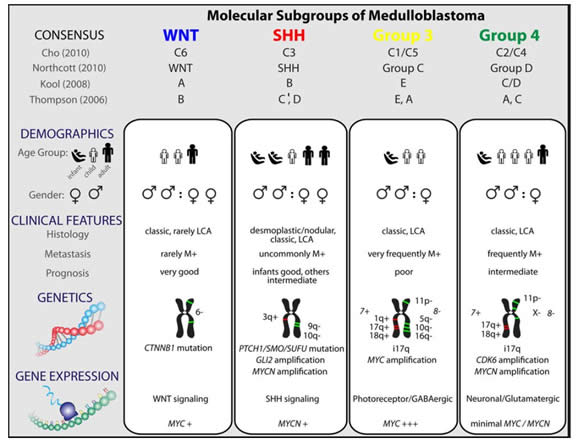
Four main subgroups of medulloblastoma identified:
1. Wnt
- Very good long-term prognosis (over 90% long-term survival)
- Accounts for less than 10% of medulloblastomas in children
- Often develop in a central location abutting the brainstem
- Occurs in older patients (median age 10yrs)
- Wnt signalling pathway aberration is related to Beta catenin mutations leading to increased protein synthesis and cell cycling
- Germ line mutations of the Wnt pathway inhibitor APC predispose to Turcot syndrome (associated with increased risk of medulloblastoma)
- Very likely to be an etiological role for canonical Wnt signaling in
the pathogenesis of these tumors - Almost all have classic histology
- Tends to occur in older children
- CTNNB1 mutations common
- Nuclear immunohistochemical staining for b-catenin common
- Monosomy six (deletion of one copy of chromosome 6 in the tumor) common
2. Shh (Sonic Hedgehog subgroup)
- Sonic Hedgehog pathway is secondary to a PTCH mutation
- Accounts for about 25% of cases
- Sonic Hedgehog signaling pathway is thought to drive tumor development in these cases:
- Gorlin syndrome = Individuals with germ line mutations in the Shh receptor PTCH and this syndrome predisposes to the development of medulloblastoma
- Germ line mutations of the Shh inhibitor SUFU also predispose to the development of medulloblastoma (especially infantile medulloblastoma)
- Shh tumors identified on the basis of transcriptional profiling
- Shh subgroup tumors have high levels of expression of MYCN
- Deletion of chromosome 9q apparently limited to Shh medulloblastomas (PTCH gene is located at chromosome 9q22)
- Frequent in infants and adults over 16 years of age, but less frequent in children
- The great majority of nodular/desmoplastic medulloblastomas belong to the Shh subgroup
- Frequently arise in the cerebellar hemisphere
- Prognosis of Shh medulloblastoma similar to Group 4 medulloblastomas (moderately good)
3. Group 3
- Mostly classic medulloblastoma histological picture
- Accounts for 25% of medulloblastoma
- High incidence of large cell/anaplastic histology
- Frequently have metastatic disease at diagnosis
- Poor prognosis
- Immunohistochemical positivity for NPR3
- Transcriptional profile that clusters with other Group 3 tumors
- Group 3 and Wnt subgroup tumors have high levels of expression of MYC
- Group 3 can be further subdivided into:
- Group 3 alpha:
- All patients with MYC amplifications and group 3 diagnosis
- high risk of recurrence and death
- Group 3 beta:
- No MYC amplifications
- Better prognosis with clinical outcome similar to Group 4 patients
- Group 3 alpha:
- Amplification and over-expression of the medulloblastoma oncogene OTX2 appears to be restricted to Group 3 and Group 4 tumors
- Group 3 tumors are much more likely than Group 4 tumors to show
gain of chromosome 1q, and/or loss of chromosome 5q and chromosome 10q
4. Group 4
- Prototype for medulloblastoma: classic histology medulloblastoma with isochromosome 17q in a 6 - 8 year old boy
- Molecular pathogenesis of Group 4 tumors unclear
- Transcriptional profile that clusters with other Group 4 medulloblastomas
- KCNA1 suggested as an immunohistochemical marker for Group 4 tumors (requires validation)
- Isochromosome 17q is also seen in Group 3 tumors (26%), but is much more common in Group 4 tumors where it is the most common cytogenetic change observed (66%)
- Tumors in 80% of females with group 4 medulloblastoma show loss of the X chromosome
Comparison of the various subgroups of medulloblastoma taken from consensus paper:
These findings need to be validated prospectively and as time goes on this classification will be refined.