Ependymoma
Prognosis
For pediatric cases alone, the 5-year overall survival rate for ependymoma is 60 - 70% if treated with attempted gross total resection and post-operative high dose RT1.
Prognostic factors can be thought of in terms of relating to the patient, the tumor and the treatment.
For localized disease the most important prognostic factor is the completeness of surgical resection. Gross total resection is associated with an improved EF and O survival.
In the table below, the most important prognostic factors are outlined in red.
Prognostic factors and their predictions for the outcome of the disease:
Prognostic Factor Category |
Factor | Outcome |
| Patient | Age | Younger patients have a worse prognosis. Children under age 3 at diagnosis are particularly at risk |
| Tumor | Tumor Extent | Metastatic tumor vs. Non-metastatic at presentation |
| Grade | Worse outcome with higher tumor grade
High-grade tumors are more often associated with craniospinal seeding |
|
| Location | Infratentorial tumors have worse prognosis than supratentorial tumors | |
| Increased risk or recurrence with brainstem invasion (neuroimaging or neurological signs) | ||
| Treatment | Surgery | Gross total resection improves both overall and progression-free survival |
| RT dose | Increased risk of occurrence with lower RT dose:
|
With aggressive approach for non-metastatic ependymoma, Event Free Survival (EFS):
- Over 75% at 7 years after gross total resection (vs 34% after incomplete resection)
- Over 75% at 7 years for grade 2 tumors (vs 60% or so for higher grade tumors)
Local control over 90% at 7 years after gross total resection and high dose conformal RT
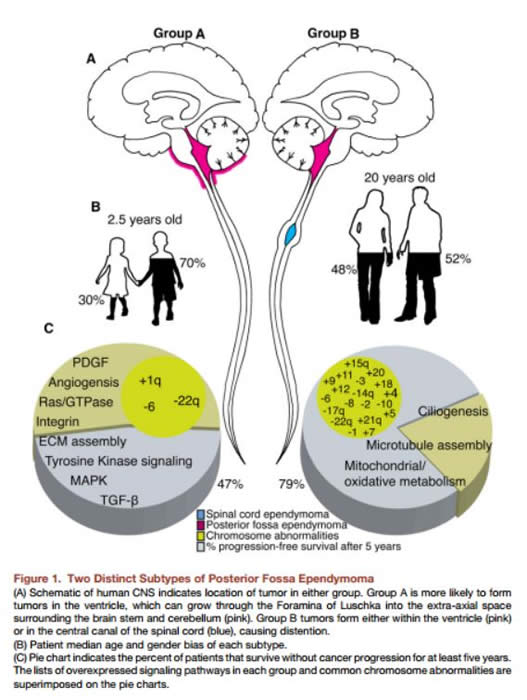
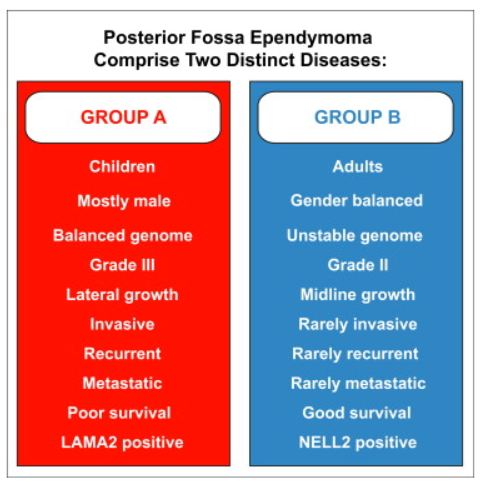
Group A and B ependymomas:
Recent research on ependymomas has identified that this tumor may be comprised of multiple, distinct entities with different characteristics. Transcriptional profiling of two large independent cohorts of ependymoma revealed the existence of two distinct groups of ependymomas.
The diagrams below are linked to the source articles: