A number of factors influence prognosis:
Local versus Metastatic
Prognosis for localized disease: EFS about 70% at 3 years (JCO 2005 Mar;23(9):2004-11).
The prognosis for patients with metastatic disease appears depends on
- Site(s)
- Number of metastases
- Surgical resectability of the metastatic disease.
Patients with metastasis to other bones distant from the primary tumor experience roughly 10% event-free and overall survival.
In patients with metastases confined to lung have an EFS about 45%. In lung prognosis appears more favorable for patients with fewer pulmonary nodules and for those with unilateral rather than bilateral pulmonary metastases
Multifocal osteosarcoma:
- Presents with symmetrical, metaphyseal lesions
- May be difficult to decide which is the primary lesion
- Multifocal bone disease at presentation has an extremely poor prognosis
- No patient with synchronous multifocal osteosarcoma has ever been reported to be cured
- Systemic chemotherapy and aggressive surgical resection may achieve significant prolongation of life
Pathology
Pathology (parosteal and intraosseous well differentiated) have a favorable prognosis.
Response to chemotherapy
Patients with more than 90% necrosis in the primary tumor after induction chemotherapy have a better prognosis than those with less necrosis (75-80% versus 45-50%).
The degree of necrosis in the primary tumor after induction chemotherapy remains prognostic in metastatic osteosarcoma.
Huvos response classification widely referred to although not used in all groups:-
Histologic Response of Osteosarcoma to preoperative chemotherapy:
I |
Little or no effect identified |
II |
Areas of acellular tumor osteoid, necrotic and/or fibrotic material attributable to the effect of chemotherapy with other areas of histologically viable tumor |
III |
Predominant areas of acellular tumor osteoid, necrotic and/or fibrotic material attributable to the effect of chemotherapy with only scattered foci of histologically viable tumor cells identified |
IV |
No histologic evidence of viable tumor identified within the entire specimen |
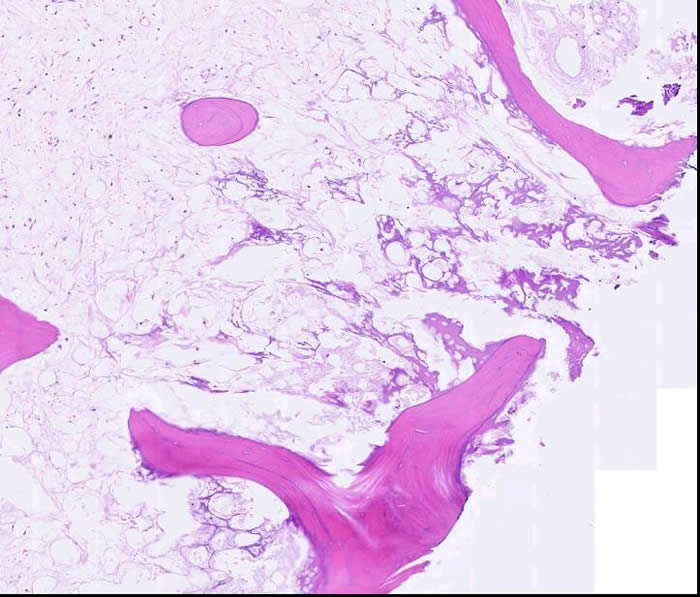
The histopathology slide below shows osteosarcoma – post neoadjuvant treatment. All tumor cells are wiped out, with only a small amount of matrix and reactive/edematous tissue remaining.
Tumor site
Among tumors of the extremity, distal sites have a more favorable prognosis than proximal sites.
Axial skeleton primary tumors:
- Greatest risk of progression and death
- Pelvic osteosarcomas make up 7% to 9% of all osteosarcomas
- Current overall survival rate is 20% to 47%
Osteosarcoma of craniofacial bones:
- Complete resection of the primary tumor with negative margins is essential for cure.
- High rate of inferior necrosis following neoadjuvant chemotherapy, BUT fewer patients with craniofacial primaries develop systemic metastases than patients with osteosarcoma in the extremities
- ? Related to the relatively smaller size and higher incidence of lower grade tumors in osteosarcoma of the head and neck.
Tumor size
Larger tumors have a worse prognosis than smaller tumors. (Inconsistent in recent literature)
Molecular Characteristics:
The significance of these factors is usually derived retrospectively and not fully validated:
- Good Prognosis:
- Lack of LOH at RB
- Absence of telomerase activity or activation of alternative lengthening of telomeres
- Poor prognosis:
- Her-2 over expression (variable consistency in literature)
- Ezrin expression (membrane cytoskeleton linkage protein)
- VEGR expression

