Pulmonary Complications
Respiratory distress is relatively common following HSCT and has a broad differential diagnosis which includes:
- Cardiogenic pulmonary edema (e.g. myocardial infarction in older patient)
- Non-cardiogenic pulmonary edema (transfusion-related acute lung injury, systemic inflammatory response syndrome).
- Iatrogenic pulmonary edema (too much IV fluids)
- Infectious pneumonia (bacterial, viral, fungal)
- Diffuse alveolar hemorrhage
- Idiopathic Pneumonia Syndrome (non-infectious)
Idiopathic pneumonia syndrome (IPS)
This is a specific early transplant complication that presents with
- Respiratory distress
- Hypoxemia
- Diffuse pulmonary infiltrates on chest X-ray.
IPS tends to occur around the time of engraftment and may be part of a greater “engraftment syndrome”.
IPS occurs because of a state of hypercytokinemia, systemic inflammation, and rapidly rising neutrophils that cluster in the lungs.
Mortality from IPS is very high (about 60%).
Treatment is supportive (intubation, mechanical ventilation).
A new experimental protocol using Etanercept (anti-TNF-a receptor antagonist) is showing promise.
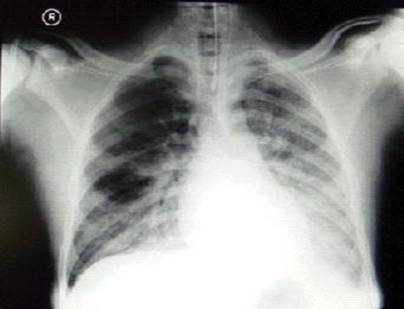
Figure: Diffuse bilateral pulmonary infiltrates in a patient with severe respiratory distress after allogeneic HSCT. Differential diagnosis is extensive. No etiology could be found including after lung biopsy and a diagnosis of IPS was made. Patient died on the ventilator.