Secondary Neoplasms
There is a significantly increased risk of second cancers of the brain, thyroid, soft tissue and bone after radiation therapy (RT).
At 25 years after diagnosis of the first malignancy treated with radiotherapy some estimates are as high as a 12% risk of a second neoplasm.
Some genetic disorders which predispose patients to their primary cancer (e.g. retinoblastoma) also in turn increase the risk of a second malignant neoplasm (SMN).
In general terms, the higher the dose of RT received, the greater the risk of a second malignancy. This is increased further by additional treatments:
- Chemotherapy
- Immune modulating treatments (e.g. BM transplant)
Younger children are more at risk. Children are more susceptible to the carcinogenic effects of radiation as their tissues are still developing as part of the normal growth process.
Studies of pediatric cancer survivors have shown up to a 22-fold excess risk of CNS neoplasms after cranial RT and chemotherapy for childhood ALL.
Patients are at risk of developing both aggressive (astrocytoma) and more indolent (meningioma) tumors.
Multiple survivorship studies continue to shed light on the magnitude of this increased risk.
- More likely to be multiple
- More likely to be atypical
- More likely to recur after resection
- NF2 mutations less likely to play a role in evolution rather than sporadic.
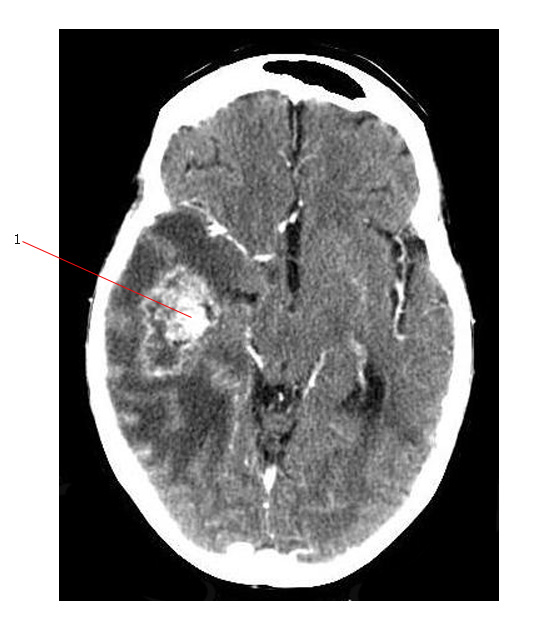
Below is a MR of a large radiation induced meningioma (#1). The patient had prophylactic cranial RT for ALL. The tumor is dural based and had most likely grown slowly and silently over many years.
Astrocytomas
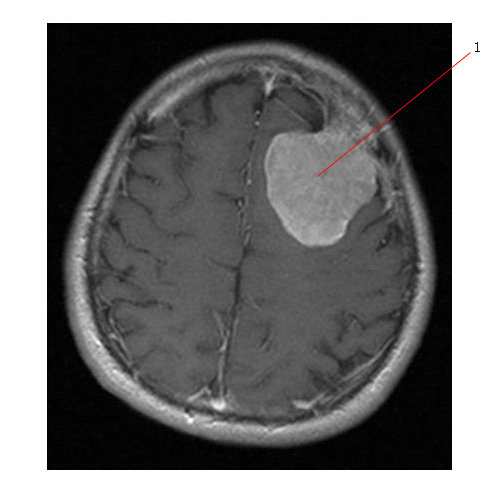
The CT scan below was done to investigate increasingly severe headaches in a patient treated with craniospinal radiotherapy for medulloblastoma 25 years earlier. There is a ring enhancing lesion (#1) in the right temporal lobe associated with significant vasogenic edema. Biopsy was positive for Glioblastoma Multiforme.