Gastro-Intestinal
Radiation Therapy (RT) Related Injury
Radiation enteritis = injury of the colon and small intestine occurring secondary to RT
Acute radiation enteritis:
- Usually have diarrhoea and abdominal pain shortly after RT therapy
- Symptoms often resolve within 3 months
- May occur after doses as low as 5–12 Gy (but usually higher doses involved)
Chronic radiation enteritis:
- Usually develops between 18 months and 6 years after completion of RT (but may occur up to 15 years after)
- Most commonly caused by:
- Inflammation and fibrosis within the wall of the GI tract. Thickening of the serosa, muscularis and submucosa leads to scarring and stenosis. The submucosa has a very rapid cell turnover and is especially vulnerable to damage.
- Enteritis or inflammation of the mucosa or lamina propria, ulceration and villous atrophy can occur independent of any fibrosis.
- Vascular changes within the mesentery may also cause ischemia in the submucosa.
Chronic radiation enteritis has been reported in up to one fifth of patients who receive pelvic RT.
Chronic enteritis is rarely seen in patients who had no acute GI toxicity at the time of therapy.
Pathological changes of chronic enteritis include:
- Obliterative endarteritis causing tissue ischaemia and necrosis
- Submucosal fibrosis
- Lymphatic dilatation
- Severe transmural fibrosis can also occur
Risk factors:
Patient related:
The risk of chronic radiation enteritis increases with the presence of co-morbid conditions:
- Diabetes, hypertension, collagen vascular diseases (as CCS age, then these conditions are likely to add to the risk of chronic bowel problems)
- Pre-existing inflammatory bowel disease
- Smoking history (in adults, but as CCS age, smoking would be very likely to increase the risk of chronic enteritis)
- Previous intestinal surgery
- Low body mass index
Treatment related:
- Dose and extent of radiation therapy. CCS who previously had treatment for large intra-abdominal or pelvic rhabdomyosarcomas are especially at risk, as these tumors often require moderately high dose RT and large fields to achieve local control.
- Previous surgery and history of adhesions are associated with a significant risk of small bowel injury at lower RT doses.
- Concurrent sensitizing chemotherapy increases the risk of RT induced damage.
Esophagus
Thoracic RT at doses of 40 Gy or more can be associated with the long term complication of esophageal stricture.
Hodgkin lymphoma patients treated with moderately high dose RT to the mediastinum 10 – 15 years ago have a 15 – 40% risk of developing this complication.
Subacute fungal infection at the time of therapy may increase the risk of this complication.
Small bowel
RT is associated with enteritis and long term fibrosis leading to strictures.
RT induced complications typically occur within 5 years of therapy (but sometimes can be as long as 20 years after therapy) and in patients who had acute GI toxicity during their cancer treatment.
Risk of RT induced injury primarily depends on:
- RT Total dose
- Treatment volume (the amount of small bowel in the RT field)
Serious enteritis is rare when total radiation doses of 50 Gy or less
are used.
TD 5/5 = The total dose at which 5% of patients would be expected to experience small bowel enteritis at 5 years:
- 50 Gy for a third of the volume of small bowel
- 40 Gy for the whole volume
TD 50/5 = The dose at which 50% of patients would develop small bowel enteritis at 5 years:
- 60 Gy for a third of the volume
- 55 Gy for the whole volume
The RT fractionation schedule does matter and it is assumed that for the above tolerances, the radiation is given in 2 Gy fraction sizes.
Clinical Picture of RT induced small bowel damage:
- Bowel obstruction secondary to adhesions
- Chronic malabsorption
- Chronic diarrhoea
- Bowel obstruction secondary to bowel stricture
- Enteric fistula formation
Large Bowel:
The large bowel is less easily damaged by RT, but can still be at risk for fibrosis and strictures.
TD 5/5 = The total dose at which 5% of patients would be expected to experience colon enteritis at 5 years:
- 55 Gy for a third of the volume
- 45 Gy for the whole volume
TD 50/5 = The dose at which 50% of patients would develop colon enteritis at 5 years:
- 65 Gy for a third of the volume
- 60 Gy for the whole volume
Irritable bowel syndrome and chronic dysmotility are common late health effects
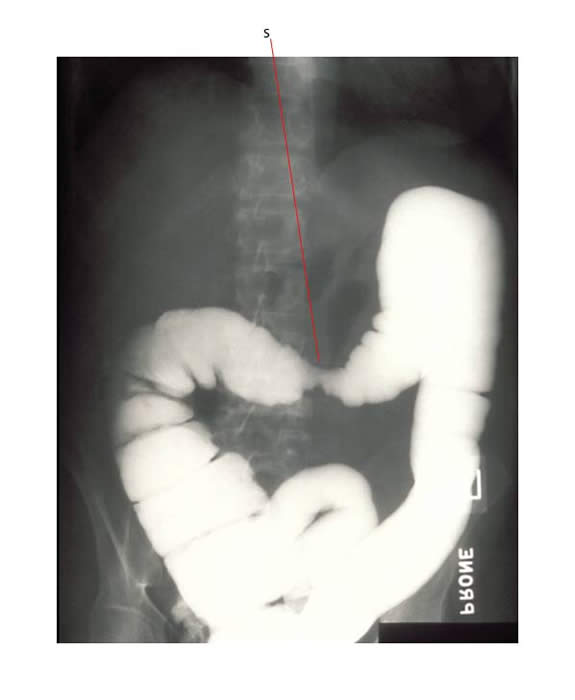
The barium study below shows a RT induced bowel stricture (S).
Rectum:
The rectal mucosa can sustain chronic RT damage with the formation of telangiectasia and a subsequent risk of rectal bleeding.
Tolerances:
The following is a table of RT tolerances for adult patients (with no allowance made for concurrent chemotherapy or bowel surgery:
- TD 5/5 means a 5% risk of complications within 5 years
- TD 50/5 means a 50% risk of complications within 5 years
Proportion of Organ in field |
TD 5/5 Gy
1/3 |
TD 5/5 Gy
2/3 |
TD 5/5 Gy
3/3 |
TD 50/5 Gy |
Injury |
Esophagus |
60 |
58 |
55 |
70 Gy |
Stricture/Perforation |
Small Intestine |
50 |
- |
40 |
Ulceration/Perforation |
|
Colon |
55 |
- |
45 |
|
Obstruction/Perforation/Ulceration/Fistula |
Rectum |
- |
- |
60 |
|
Severe proctitis/Necrosis/Fistula/Stenosis |
Second cancers:
RT increases the risk for the development of second cancers involving the GI tract. RT to the abdomen, pelvis or spine is likely to be associated with an increased risk of colo-rectal cancer (CRC).
Factors which significantly increase the risk of CRC include a previous history of:
- RT doses of 30 Gy or higher to the abdomen, pelvis, or spine
- Large volume RT
- Chemotherapy that included alkylating agents (e.g. cyclophosphamide)
Reference:
Secondary Colorectal Carcinoma After Childhood Cancer
Kerri Nottage, Joshua McFarlane, Matthew J. Krasin, Chenghong Li, Deokumar Srivastava, Leslie L. Robison and Melissa M. Hudson
This study demonstrated a radiation dose-response effect on the risk of colo-rectal cancer (CRC) with a 70% increase in risk for every10 Gy increase in dose. A greater volume of tissue irradiated, as estimated by number of colonic segments in the radiation field, imparted 1.5 and 1.8X the risk per segment of developing CRC.
In addition Alkylating agent exposure was associated with an 8.8X increased risk of secondary CRC.
Some CRC cases in this analysis developed in survivors treated with less than 30 Gy of abdominal RT - therefore the dose threshold for surveillance should perhaps be
re-evaluated.

