Informed Consent
Introduction
Effective informed consent means effective communication between the health care practitioner (HCP) and patient.
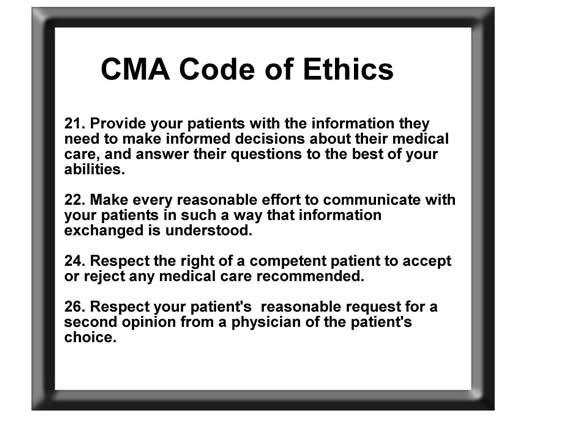
The Canadian Medical Association Code of Ethics contains specific recommendations regarding decision making and informed consent:
Foundation of Informed Consent
The historical basis of law which attempted to ensure informed consent originally was legal liability for assault and battery (non-consensual touching).
The touching, not the result is the battery. The patient may have actually benefited from “the touching” - though in the first case documented about informed consent, this seems doubtful.
First informed consent case: Slater v Baker (English case, 1767)
A physician first set the patient’s femoral fracture in accordance with practice at the time, but in follow up, he forcibly re-broke the bone and placed the re-broken bone in a mechanical device with teeth.
Physicians brought to court testified that it was usual for a physician to secure their patient’s consent before a medical intervention.
The judge ruled that consent should have been obtained.
“It is reasonable that patient should be told what is about to be done to him.”
Judge also ruled that procedure was out of the ordinary and other doctors would not have used this method, but little was said about the fact that this was an experimental intervention.
Battery vs. Negligence
Over time negligence theory has replaced common law battery as a basis for litigation.
Battery theory of liability would be very rarely used. Only if:
- No consent at all was given then it would be possible to use battery theory to impose liability on a Health Care Professional (HCP) – but this would be very unusual.
- Procedure performed which was completely or substantially different from the one authorized.
Supreme Court of Canada has “located” the duty to inform within the law of negligence.
The Term "Informed Consent"
There are many reasons why “informed consent” is not the best term, including:
- Does not cover informed refusal
- Implies that the purpose of giving information is only to obtain consent for a procedure
- Only benefit is to protect medical practitioner
“Informed decision making” is a better term.